Introduction
Hello and welcome to our exploration of a very significant topic in child mental health – the impact of early stimulant treatment on brain structure in ADHD. Attention-Deficit/Hyperactivity Disorder, or ADHD, is a condition we’ve all heard about. It’s quite prevalent, affecting millions of children and often continuing into adulthood. The journey of understanding and managing ADHD is not just a clinical one; it’s deeply personal for many families and individuals.
As a psychiatric mental health nurse practitioner, I’ve seen firsthand how early diagnosis and intervention can make a world of difference. Imagine a young boy, let’s call him Alex, struggling in school, unable to sit still, and often being labeled as ‘troublesome’. When Alex was diagnosed with ADHD and began treatment, it wasn’t just his behavior that started to change; it was as if his entire world opened up. Suddenly, he could focus, engage, and even excel in ways no one expected. This transformation is not just about managing symptoms; it’s about unlocking potential.
Stimulant medications, like methylphenidate and amphetamines, are common in treating ADHD. They have been the subject of extensive research and discussion. The focus of this article, however, is a bit more specific. We’re diving into how these treatments, especially when started early, can impact the brain’s structure. It’s a fascinating area that combines neurology, psychiatry, and a deep understanding of human development.
Why focus on brain structure, you might ask? Well, the brain is an amazing organ, constantly evolving, especially in children. In ADHD, this development can be quite unique, and understanding it is key to effective treatment.
So, whether you’re a parent, a healthcare professional, or just someone interested in learning more about ADHD, I invite you to join me on this insightful journey. We’ll explore what ADHD really is, how stimulant medications work, and most importantly, how early intervention can shape not just behavior, but the very structure of the brain itself. Let’s demystify some of the common misconceptions and fears, and equip ourselves with knowledge, because, as the saying goes, knowledge is power. And in the case of ADHD, it’s the power to transform lives.
Understanding ADHD
So, let’s dive into what ADHD really is. Imagine being in a room where the TV, radio, and computer are all on at full volume. That’s a day in the life of someone with ADHD. It’s not just about being hyperactive or inattentive; it’s about navigating a world of overwhelming stimuli. ADHD, or Attention-Deficit/Hyperactivity Disorder, is a neurodevelopmental disorder characterized by symptoms like difficulty focusing, hyperactivity, and impulsive behavior.
Now, there are quite a few myths about ADHD. Some people think it’s just kids being kids, or worse, a result of poor parenting. But trust me, as someone who’s worked with countless families, ADHD is as real as any other medical condition. It’s not about bad behavior or a lack of discipline. It’s about the brain working differently.
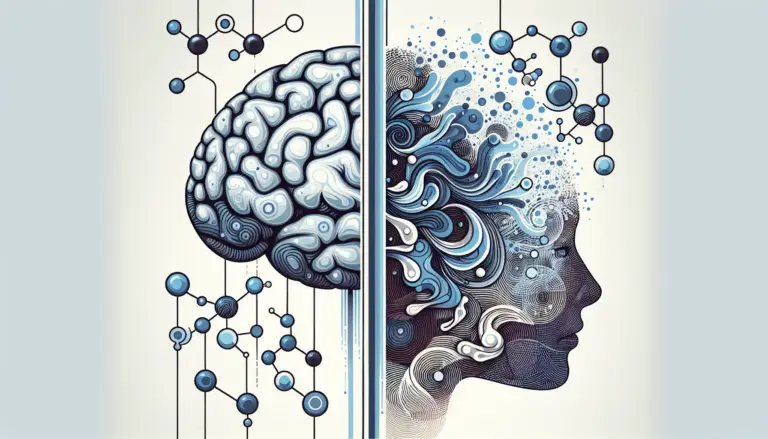
Speaking of the brain, let’s talk about how ADHD affects it. Research shows that ADHD is linked to the development and function of certain brain areas. These areas are responsible for things like attention, impulse control, and planning. In children with ADHD, these parts of the brain may develop more slowly or function differently. This doesn’t mean they’re less intelligent or capable – far from it. It just means their brains process information differently.
I remember one of my young patients, Sarah, who had a hard time in school because she couldn’t sit still or focus. Her parents were frustrated and felt helpless. But once they understood that Sarah’s brain works in its unique way, they became her biggest advocates. They learned strategies to help her focus and tailored her learning environment to her needs. Sarah’s story is a powerful reminder of why understanding ADHD is crucial.
Early childhood is a critical time for brain development. That’s why addressing ADHD during this stage is so important. Early intervention can help shape the brain’s development and set the foundation for future learning and behavior patterns.
As we explore ADHD further, remember, it’s not about a lack of willpower or intelligence. It’s about understanding and supporting a brain that functions differently. And by doing so, we can help individuals with ADHD not just survive, but thrive.
Stimulant Medications for ADHD
Now, let’s chat about a key player in the ADHD treatment game: stimulant medications. You’ve probably heard of some of these, like methylphenidate or amphetamines. They sound a bit intimidating, right? But let me assure you, when used correctly, they can be incredibly effective.
Here’s a little science behind how these medications work. Contrary to what their name might suggest, stimulants don’t just ‘stimulate’ the brain randomly. They actually increase the availability of certain neurotransmitters, like dopamine and norepinephrine. These are like the brain’s messengers that help with attention and focus. In a way, stimulants help turn up the volume on the brain’s messaging system, making it more efficient for someone with ADHD.
But what does this look like in real life? Picture this: a child who used to be easily distracted in class, constantly fidgeting, and struggling with homework, starts to show remarkable improvements with medication. They can follow a lesson, participate without disrupting, and complete tasks they previously couldn’t. It’s not magic; it’s medicine at work.
Now, I’ve had parents express concerns about medicating their child. It’s a valid worry. No one wants to see their child become a different person or deal with a bunch of side effects. But here’s the thing – when used under proper medical guidance, these medications can improve the quality of life significantly. They’re not about changing who the child is; they’re about helping them be their best selves.
Of course, it’s not a one-size-fits-all solution. Finding the right medication and dosage can be a process. I recall a young teenager, Emily, who we started on a low dose of medication. It took a few adjustments to find the sweet spot where she felt ‘just right.’ This journey is common and a crucial part of finding the most effective treatment.
The benefits of stimulant medications for ADHD are well-documented. They can help improve focus, reduce impulsivity, and even enhance social interactions. But it’s important to remember that medication is often just one part of a comprehensive treatment plan that includes therapy, lifestyle changes, and educational support.
In summary, stimulant medications can be a game-changer for many with ADHD. They’re not about doping up or numbing down; they’re about empowering individuals to navigate their world more effectively. As we move forward, keep in mind that the goal of any treatment, medication or otherwise, is to enable individuals with ADHD to harness their unique strengths and lead fulfilling lives.
Early Intervention and Its Importance
Alright, let’s talk about why timing is everything when it comes to ADHD. Early intervention – it’s a phrase we hear a lot, but what does it really mean? Essentially, it’s about recognizing and addressing ADHD as soon as possible. And trust me, the ‘early’ part is crucial.
Think of the brain like a garden. In early childhood, it’s like fertile soil, ready to be shaped and nurtured. When ADHD is identified and treated early, we’re essentially helping to guide the growth of this garden, ensuring that the right pathways are developed. This can have a ripple effect on a child’s entire future.
The benefits of early intervention are huge. It can lead to better outcomes in school, improved relationships, and a more positive self-image. It’s like giving a child a head start in a race they’ll be running their whole life.
But it’s not always easy. Diagnosing ADHD in young children can be challenging. They’re naturally energetic and easily distracted – it’s part of being a kid, right? So, when does it cross the line into ADHD? This is where skilled professionals come in. It’s a delicate balance, understanding the difference between typical childhood behavior and something that might need a little extra attention.
I remember a little guy named Lucas. He was so full of life, always on the move, a real whirlwind. His parents were worried he was ‘too much’ for his teachers and classmates. When Lucas was diagnosed with ADHD and started treatment, the change was not just in his ability to sit still but in his ability to connect with the world around him. His parents were relieved, and Lucas felt more confident.
There are challenges, of course. Some parents worry about labeling their child or relying on medication. But early intervention isn’t about labels or quick fixes. It’s about understanding and supporting a child’s unique needs.
When we catch ADHD early, we’re not just putting out fires; we’re building a stronger, more resilient foundation. And that’s something that can benefit a child for their entire life.
So, as we continue our journey through understanding ADHD, let’s remember the power of early intervention. It’s not just about addressing challenges; it’s about nurturing potential and helping every child to bloom in their own unique way.
Impact of Early Stimulant Treatment on Brain Structure
Now, let’s delve into something truly fascinating – the impact of early stimulant treatment on the brain structure of those with ADHD. This is where science really gets exciting!
When we talk about ADHD, we’re not just talking about behavior; we’re talking about the brain. Specifically, how certain parts of the brain develop and function. What’s really intriguing is how early treatment with stimulants can actually influence this development.
Here’s the scoop: recent research has shown that stimulant medications can affect areas of the brain involved in attention, impulse control, and executive functioning. These are the parts of the brain that can be a bit sluggish in individuals with ADHD. MRI studies showed lower gray matter density, white brain matter abnormalities, lower total brain volume, slower maturation of certain areas, and reduced thickness and size of some areas. But with early treatment, these areas can develop more typically. It’s like giving the brain a gentle nudge in the right direction.
Picture this: two children, both with ADHD, but only one starts early treatment with stimulants. Over time, studies suggest that the child who received early treatment might show more typical brain development patterns compared to the one who didn’t. It’s not about “curing” ADHD; it’s about giving the brain the support it needs to grow and function at its best.
I recall a teenager, Jake, who started on stimulant medication at a young age. When he was younger, he struggled a lot with impulse control and getting along with others. Fast forward to after years of treatment, and Jake was not just managing his ADHD; he was thriving. His ability to focus and regulate his behavior had improved dramatically. It was a clear testament to how early intervention can make a long-term difference.
Now, it’s important to understand that this isn’t a one-size-fits-all situation. Every brain is unique, and so is every case of ADHD. But what these findings give us is hope – hope that early, appropriate treatment can do more than just manage symptoms; it can potentially shape the brain’s development in a positive way.
Of course, there’s still much to learn. But as we continue to research and understand ADHD, we’re finding more and more evidence that early intervention – especially with stimulant medications – can have a profound impact on the brain. And that’s not just exciting for scientists and doctors; it’s life-changing for individuals with ADHD and their families.
Addressing Concerns and Misconceptions
Let’s tackle a really important part of our conversation about ADHD and stimulant medication: addressing concerns and busting some myths. It’s natural to have questions and worries, especially when it comes to something as complex as brain health and medication.
First off, a big concern for many parents is the idea of side effects from stimulant medications. It’s true, like any medication, stimulants can have side effects. Some kids might experience things like decreased appetite or trouble sleeping, especially when they first start the medication. But here’s the key – these side effects are often manageable and tend to decrease over time. It’s all about finding the right balance, which can take a bit of trial and error.
I remember a conversation with a mom, let’s call her Mrs. Smith, who was really worried about starting her son on medication. “Will he still be himself?” she asked. This is a common fear. But here’s the thing: the goal of ADHD treatment is not to change a child’s personality. It’s about helping them be their best selves. Mrs. Smith’s son, once he started on the right medication, was still the vibrant, fun-loving kid he always was, but now he could channel his energy and focus better.
Now, let’s debunk a big myth: “Stimulant medications are just a way to sedate kids with ADHD.” This couldn’t be further from the truth. Stimulants don’t sedate; they help balance neurotransmitters in the brain, which can improve focus and reduce impulsivity and hyperactivity.
Another concern is about the long-term impact of taking stimulants. The good news is, decades of research have shown that when used as prescribed, these medications are generally safe in the long term. Of course, every child is different, and ongoing monitoring by a healthcare professional is essential.
It’s also worth noting that medication is often most effective when combined with other therapies, like behavioral therapy, counseling, or educational support. It’s not a standalone solution, but part of a comprehensive approach to managing ADHD.
In essence, addressing ADHD with stimulant medication is about creating an environment where kids can flourish. It’s about giving them the tools they need to navigate their world more effectively. And as we continue to learn and grow in our understanding of ADHD, we’re finding more ways to help these amazing kids shine in their own unique way.
Case Studies and Real-life Examples
Alright, let’s bring our discussion to life with some real-world stories. Case studies and personal experiences can really illuminate how early stimulant treatment impacts those with ADHD. These are not just clinical anecdotes; they’re snapshots of real journeys, full of challenges, triumphs, and invaluable lessons.
First, let’s talk about Emma, a bright 8-year-old with a sparkle in her eyes and energy to match. When Emma first came to my office, she was struggling in school, often feeling overwhelmed and “out of sync” with her classmates. After a careful evaluation, Emma was diagnosed with ADHD. We started her on a low dose of a stimulant medication. The change didn’t happen overnight, but over time, Emma’s mom reported amazing progress. Emma began to participate more in class, her grades improved, and most importantly, her self-esteem soared. It was like watching a flower bloom in fast forward.
Then there’s the story of Daniel, a 10-year-old who loved soccer but couldn’t stay focused enough to follow the coach’s instructions. After starting stimulant treatment, Daniel’s parents and coach noticed a remarkable difference. He was more attentive during practice and games, and his social interactions with teammates improved. This wasn’t just about better soccer skills; it was about Daniel feeling more connected and successful in something he loved.
These stories echo what I hear from many other healthcare professionals. A colleague of mine shared a story about a teenager, Lily, who struggled with severe impulsivity and disorganization due to her ADHD. With early intervention, including stimulant medication and cognitive-behavioral therapy, Lily transformed during her high school years. She went from being at risk of failing to being an honor roll student and an active participant in school clubs.
But it’s not always a smooth road. Adjusting to medication can take time, and every child’s response is unique. I recall a young boy, Bobby, who went through several medication adjustments before finding the right fit. His journey reminds us of the importance of patience and perseverance in ADHD treatment.
These stories are more than just clinical successes. They’re about children and teenagers who found new paths to expressing their talents, connecting with others, and realizing their potential. They highlight the multifaceted nature of ADHD treatment – it’s not just about managing symptoms, but about nurturing growth, confidence, and resilience.
So, as we discuss the nuts and bolts of ADHD and its treatments, let’s not forget the human side of the story. Behind every case study are real kids with dreams, challenges, and the incredible capacity to grow and thrive.
Looking Ahead: Future Research and Developments
As we near the end of our journey through the world of ADHD and early stimulant treatment, let’s take a moment to gaze into the future. What does it hold for ADHD research and treatment? Spoiler alert: it’s pretty exciting!
First off, there’s a ton of ongoing research diving deeper into how ADHD affects the brain and how treatments like stimulants can help. We’re learning more every day about the intricacies of the brain and how ADHD plays out in its complex landscape. This means we’re getting closer to even more personalized and effective treatments.
One of the hot topics in ADHD research is neuroplasticity – that’s the brain’s amazing ability to change and adapt. Scientists are exploring how early treatment might influence this neuroplasticity, potentially leading to long-lasting positive effects. Imagine treatments that don’t just manage symptoms, but fundamentally help the brain develop in more typical ways. That’s the dream, and we’re getting closer to it.
There’s also a growing interest in non-medication treatments and how they can complement traditional therapies. Things like cognitive-behavioral therapy, mindfulness, and lifestyle changes are getting more attention. It’s all about a holistic approach – treating the whole person, not just the ADHD symptoms.
And let’s not forget about technology. With advancements in digital health and telemedicine, access to care and ongoing support for ADHD is becoming more convenient and personalized. We’re seeing apps and online programs designed to help with organization, time management, and even mindfulness exercises specifically for ADHD.
The future of ADHD treatment is also likely to be more inclusive and diverse. We’re recognizing the importance of understanding how ADHD presents in different genders, ethnicities, and backgrounds. This means better, more tailored care for everyone.
So, what does all this mean for you? Whether you’re a parent, a person with ADHD, or just someone interested in the topic, the future is bright. We’re moving towards a world where ADHD is understood more deeply, treated more effectively, and where individuals with ADHD are supported in realizing their full potential.
In conclusion, the field of ADHD is evolving rapidly, and the prospects are exciting. We’re not just looking at managing a condition; we’re looking at transforming lives. The journey of understanding and treating ADHD is an ongoing one, full of discoveries and advancements. And the best part? We’re all part of this journey, contributing to a future where every individual with ADHD can thrive.
Conclusion
Well, here we are at the end of our enlightening journey through the world of ADHD and the impact of early stimulant treatment. It’s been quite an adventure, filled with insights, real-life stories, and a glimpse into the future of ADHD care.
Let’s wrap things up by revisiting the key takeaways from our discussions:
- ADHD is More Than Meets the Eye: Remember, ADHD isn’t just about being hyperactive or distracted. It’s a complex neurodevelopmental disorder that affects the brain in unique ways. Understanding this is the first step in effective treatment and support.
- The Power of Early Intervention: We’ve seen how crucial early diagnosis and treatment are. Like nurturing a young plant, early intervention can help shape the development of a child’s brain, setting the stage for success in various aspects of life.
- Stimulants: A Key to Unlocking Potential: Stimulant medications, when used under proper medical guidance, can be a game-changer. They’re not about changing who a child is; they’re about helping them harness their inherent strengths and abilities.
- Every Child’s Journey is Unique: ADHD affects each person differently, and so does treatment. Personalized care, patience, and perseverance are essential. The stories of Emma, Daniel, Lily, and Bobby remind us of the diverse paths and possibilities in managing ADHD.
- Looking Forward with Hope: The future of ADHD treatment is bright and promising. With ongoing research, advancements in technology, and a deeper understanding of ADHD’s nuances, we’re moving towards more effective and inclusive approaches.
As we conclude, I hope this article has not only informed you but also inspired you. Whether you’re a parent navigating this journey with your child, a healthcare professional dedicated to supporting your patients, or someone with ADHD yourself, know that you’re not alone. The path of understanding and managing ADHD is filled with support, hope, and endless possibilities.
In the world of ADHD, every challenge is an opportunity to learn and grow. It’s about celebrating the unique ways in which each mind works and supporting every individual in reaching their full potential. So, let’s continue to embrace this journey with knowledge, compassion, and an unwavering commitment to nurturing young minds.
Thank you for joining me on this exploration. Here’s to a future where every individual with ADHD thrives, supported by a world that understands and values their unique contributions.
References and Further Reading
As we close the curtain on our deep dive into ADHD and the wonders of early stimulant treatment, I want to leave you with some resources to keep the learning going. Knowledge is a powerful tool, especially when it comes to navigating the complexities of ADHD.
Here’s a curated list of references and further reading materials. Whether you’re a parent, educator, healthcare professional, or just someone with a keen interest in ADHD, these resources will provide you with a wealth of information and insights.
- Academic Journals and Research Papers: For those who love to get into the nitty-gritty of science, there are numerous journals that publish the latest ADHD research. Journals like ‘Journal of Attention Disorders’ and ‘ADHD Attention Deficit and Hyperactivity Disorders’ are great places to start.
- Books for a Deeper Understanding: There are several insightful books out there. “Driven to Distraction” by Edward M. Hallowell and John J. Ratey is a classic. For a more recent take, check out “ADHD 2.0” by the same authors.
- Websites for Continuous Learning: Websites like ADDitude Magazine (additudemag.com) offer a wealth of articles, tips, and real-life stories. The CDC’s ADHD page (cdc.gov/ADHD) is also a great resource for understanding the basics and finding links to more detailed information.
- Podcasts and Webinars: For learning on the go, there are numerous ADHD-related podcasts and webinars. They feature experts, researchers, and real-life stories, providing both information and inspiration.
- Support Groups and Forums: Sometimes, the best insights come from those who are walking the same path. Online forums and local support groups can be invaluable resources for sharing experiences, tips, and encouragement.
- Apps and Tools: In our tech-savvy world, there are apps designed to help manage ADHD symptoms, like organization and time management tools. Exploring these can be both fun and beneficial.
Remember, the journey of understanding ADHD is ongoing. These resources are just a starting point. As you delve deeper, you’ll find a community of support and a wealth of knowledge. So keep learning, keep exploring, and most importantly, keep nurturing those young minds.
And there you have it – your toolkit for continuing the journey in understanding and managing ADHD. Here’s to a world where every mind is appreciated for its unique brilliance, and every individual with ADHD is empowered to reach their highest potential. Happy reading, listening, and exploring!
Glossary of Terms:
-
- ADHD (Attention-Deficit/Hyperactivity Disorder): A neurodevelopmental disorder characterized by inattention, hyperactivity, and impulsivity.
- Stimulant Medications: A type of medication used to treat ADHD, which helps increase attention and focus.
- Neurotransmitters: Chemicals in the brain that transmit messages between nerve cells.
- Neuroplasticity: The brain’s ability to adapt and change in response to experiences.
- Cognitive-Behavioral Therapy (CBT): A type of therapy that helps in changing negative thought patterns and behaviors.
- Frequently Asked Questions (FAQs):
- Q: Can ADHD be cured? A: ADHD is a lifelong condition, but its symptoms can be effectively managed with the right treatment plan.
- Q: Are stimulant medications safe for children? A: Yes, when prescribed and monitored by a healthcare professional, stimulant medications are safe and effective for children.
- Q: How can I support a child with ADHD at home? A: Establishing a routine, creating a supportive and structured environment, and using positive reinforcement can be very helpful.
- Q: Will my child outgrow ADHD? A: While some children may see a decrease in symptoms as they grow, many continue to experience ADHD symptoms into adulthood.
- Q: Is ADHD only about having trouble paying attention? A: No, ADHD also involves challenges with hyperactivity and impulsivity.
This appendix is just a small part of the vast resources available on ADHD. It’s a starting point for those seeking to understand more, and a quick reference for anyone needing a refresher.
Remember, knowledge is a powerful ally. Whether you’re a parent, teacher, healthcare provider, or someone with ADHD, the more you know, the better equipped you’ll be to navigate the challenges and celebrate the successes. So keep this appendix handy, and let it be a beacon guiding you through the fascinating and rewarding journey of understanding and supporting those with ADHD.
And with that, we close our comprehensive exploration of ADHD and early stimulant treatment. May this journey be just the beginning of a deeper understanding, greater empathy, and continued advocacy for those with ADHD. Here’s to nurturing every young mind with care, knowledge, and unwavering support!